Does Menopause Cause Joint Pain?
Contents Show
Menopause marks the end of a woman's menstrual cycles, diagnosed after 12 months without a period. It's a natural biological process, but it can lead to various physical symptoms…
So yes menopause can cause joint pain.
Understanding why menopause can cause joint pain and how to manage it is crucial for improving quality of life during this transition.
We’ll delve into the causes, symptoms, and effective relief methods for menopause-related joint pain.
How Can Menopause Affect Your Bones and Joints?
During menopause, the decline in estrogen levels can lead to decreased bone density, which is a condition known as osteoporosis.
Research shows there can be up to 20% of bone loss during the stages of menopause. (1)
This makes bones more fragile and increases the risk of fractures, and joints can suffer too.
Lower estrogen levels are linked to increased inflammation, which can exacerbate joint pain and stiffness. (2)
So during menopause, you may experience more joint pain and find your joints feel stiffer and less flexible.
Related article: Understanding the stages of menopause and their impact on your body.
What Are Common Symptoms of Menopause-Related Joint Pain?
Common symptoms include aching or soreness in the joints, which might be more pronounced in the morning.
You may also notice swelling in your joints, making them feel stiff and limiting your range of motion.
You may have a feeling of "creakiness," where joints make a cracking sound with movement.
The pain can be intermittent or constant and might vary in intensity.
Experiencing these symptoms alongside other menopausal changes, such as hot flashes or irregular periods, can be a strong indicator that your joint pain is related to menopause.
Are There Any Specific Joints That Are More Affected During Menopause?
The knees, hands, and hips are among the most commonly affected areas.
The knees, bearing much of your body's weight, can be particularly prone to discomfort and inflammation.
Hands and fingers might experience stiffness and swelling, making daily tasks more challenging.
Hip joints, too, can suffer, with pain sometimes radiating to the thighs or buttocks.
There is plenty you can do though.
When we work with our female clients who mention they have knee pain we go through a full injury screening process.
You will be amazed what strengthening the muscles around the knee, foam rolling the muscles around the knee, and doing this for a few minutes every day consistently can do for you.
Not all joint pain may be menopause related.
What Lifestyle Changes Can Help Manage Menopause-Induced Joint Pain?
Maintaining a healthy weight is crucial. Excess weight puts additional pressure on your joints, particularly the knees and hips
Incorporating regular, low-impact exercises such as walking, swimming, or yoga can improve joint flexibility and strength without exacerbating pain
A diet rich in anti-inflammatory foods, like omega-3 fatty acids found in fish and antioxidants in fruits and vegetables, can also help manage inflammation and alleviate pain
Staying hydrated and ensuring adequate calcium and vitamin D intake are important for bone health
Practicing stress-reduction techniques like meditation or deep-breathing exercises can have a positive effect on overall well-being and pain levels
How Do Hormonal Changes During Menopause Contribute to Joint Pain?
When estrogen levels drop, this can lead to an increase in inflammatory processes in the body. This can affect the joints and cause pain and stiffness.
A decrease in estrogen can lead to decreased lubrication in the joints, contributing to discomfort and stiffness.
Related article: The role of magnesium in managing menopause symptoms.
Can Hormone Replacement Therapy (HRT) Help with Joint Pain During Menopause?
By supplementing the body's declining estrogen levels, HRT can help reduce inflammation and improve joint health.
Women who use HRT may experience less severe joint pain compared to those who do not. (3)
It's important to approach HRT with a balanced view, considering its benefits against potential risks.
If you're considering HRT for menopause-related joint pain, discuss it with your healthcare provider. They can help you weigh the risks and benefits based on your health profile and preferences.
Related article: How regular physical activity can alleviate menopause-related joint pain.
Are There Alternative Treatments for Menopause-Related Joint Pain?
Natural remedies, such as collagen, herbal supplements including black cohosh and evening primrose oil, have been suggested to help with menopausal symptoms.
You should still consult with a healthcare provider for advice specific to your situation.
- Available in Unflavored, Strawberry Lemonade, Tropical Punch, Tropical Punch w/ Caffeine, Chocolate Swirl
- One-time purchase at $59.99 or subscribe & save 20% for $47.99 with free shipping
- 60-Day Money-Back Guarantee**: Ensures customer satisfaction
- Third-party verification for quality assurance
- Manufactured in the USA: Ensures product integrity and quality
- Free US Shipping: On all orders, enhancing customer convenience
Related article: The benefits of collagen supplements during menopause.
Acupuncture is another alternative therapy that some women find beneficial for managing joint pain and menopausal symptoms.
Physical therapies, including physiotherapy and chiropractic care, can also provide relief by improving joint mobility and reducing pain.
Additionally, mindfulness practices like yoga and meditation can help manage the stress that might exacerbate joint pain.
How Can Physical Activity Impact Joint Health During Menopause?
Engaging in regular physical activity is paramount for maintaining joint health during menopause.
Exercise helps strengthen the muscles around the joints, which can reduce joint strain and pain.
Activities such as walking, swimming, and cycling are excellent low-impact options that provide the benefits of exercise without putting too much stress on your joints.
Strength training, when done properly, can also be particularly beneficial for supporting joint health by building muscle mass and bone density.
We get a lot of our clients using resistance bands to start with. It’s a great way to challenge the body from the comfort of your own home.
It’s so easy to set the up, its a safe way of training, and its super super low cost.
You can get a set of bands for less than $40 (£35) and they’ll probably last you about 5-6 months before you need to replace them.
Compare that to the price of a set of dumbbells and well… it really is a no-brainer.
We use these in our own sessions too and cannot recommend them enough.
Resistance bands we recommend for our US readers
Resistance bands we recommend for our UK readers
Yoga and Pilates is great too. They not only improve flexibility and balance but also contribute to stress reduction, which can indirectly alleviate joint pain.
Incorporating a balanced mix of aerobic, strength, and flexibility exercises into your routine can have a profound impact on managing joint pain during menopause.
What Role Does Diet Play in Managing Joint Pain During Menopause?
Diet plays a huge role in managing joint pain during menopause.
Eating a balanced diet rich in anti-inflammatory foods can help reduce joint inflammation and pain.
Foods high in omega-3 fatty acids, such as salmon, flaxseeds, and walnuts, are known for their anti-inflammatory properties.
Fruits and vegetables, particularly those rich in antioxidants like berries, spinach, and carrots, can also help combat inflammation.
We recommend limiting the intake of processed foods, sugars, and red meat, which increases your inflammation…
And this the same recommendations for any client we work with where they’re going through the menopause of not.
Staying hydrated is essential as well, as water helps maintain the lubrication of your joints.
Related article: Exploring the best supplements for easing menopause symptoms in the UK.
When Should You Consult a Doctor About Menopause-Related Joint Pain?
You should consider consulting a doctor about menopause-related joint pain if:
The pain is severe and significantly impacts your daily life
Over-the-counter pain relief and lifestyle changes don't bring relief
You experience swelling, redness, or warmth around the joints
The joint pain is accompanied by other concerning symptoms, such as unexplained weight loss, fever, or fatigue
What Supplements Help Menopause Joint Pain?
Supplements such as omega-3 fatty acids, glucosamine, chondroitin, and Vitamin D have been suggested to help alleviate joint pain in menopausal women.
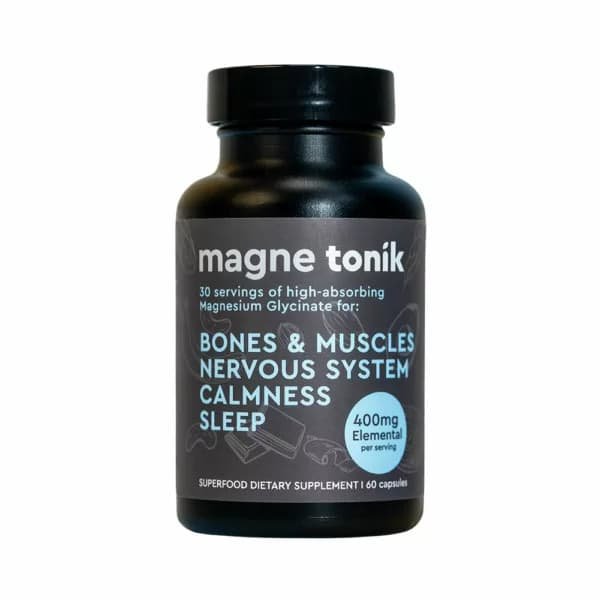
Magnesium can also be beneficial for its anti-inflammatory properties.
However, it's crucial to consult with a healthcare provider before starting any supplements, as they can interact with other medications and conditions.
- Magnesium Bisglycinate 400 mg: High-dosage magnesium supplement designed for optimal absorption, gentle on digestion
- 6 Tubs (180 days supply) for $147, saving $51
- 3 Tubs (90 days supply) for $87, saving $12
- 1 Tub (30 days supply) for $33
- Offers a 365-day money-back guarantee
- Made in the USA and 3rd Party Tested for quality assurance
Conclusion
We've explored how lifestyle changes, such as incorporating a balanced diet rich in anti-inflammatory foods and engaging in regular, low-impact exercise, can play a crucial role in alleviating joint pain.
Alternative treatments and the potential benefits of Hormone Replacement Therapy (HRT) offer additional avenues for relief, though they should be considered carefully in consultation with healthcare professionals.
The severity and experience of menopause-related joint pain vary widely among individuals.
It's important to listen to your body and seek medical advice when symptoms are severe or persistent.
With the right management strategies, it's possible to mitigate the impact of menopause on your joints and maintain an active, fulfilling life during this transition.